Navigating medical billing denials often feels like decoding a secret language. You submit a claim, confident the service was provided and documented, only to have it rejected with a vague reason. Among these frustrating codes, the CO-253 denial code stands out for its specificity and its direct link to a common billing error. If you are struggling with this denial, you are not alone.
This comprehensive guide will demystify the CO-253 denial code for you. We will break down exactly what it means, why it happens, and most importantly, provide a step-by-step action plan to resolve it quickly and prevent it from recurring. By understanding the root cause of these denials, your practice can significantly boost its clean claims rate and protect its revenue stream.
What Exactly is the CO-253 Denial Code?
In simple terms, the CO-253 denial code means: “Procedure code inconsistent with modifier.”
When a payer returns your claim with this reason, they are essentially telling you that the CPT or HCPCS code you billed does not logically pair with the modifier you attached to it. The insurance company’s claims processing system has built-in rules called “edits.” These edits check for correct coding relationships. When your code-modifier combination flags one of these edits, the system automatically denies the claim with a CO-253.
It is crucial to understand that this is a technical denial, not necessarily a judgment on medical necessity. The issue lies in the billing syntax, not always the service itself.
How is CO-253 Different from CO-24?
Many billers confuse CO-253 with the CO-24 denial code. While both relate to claim issues, they are fundamentally different. Understanding this distinction is key to an efficient resolution.
-
CO-253 (Procedure code inconsistent with modifier): This is a coding and billing error. The problem is the combination of numbers and letters on the claim form itself. The fix involves correcting the codes or modifiers.
-
CO-24 (Charges not medically necessary): This is a clinical documentation or medical necessity issue. The payer believes the diagnosis codes (ICD-10) do not justify the service performed. The fix requires providing more robust clinical notes from the medical record.
In short, CO-253 is about “how you billed it,” while CO-24 is about “why you did it.” You resolve CO-253 in your billing software; you resolve CO-24 with your clinical documentation.
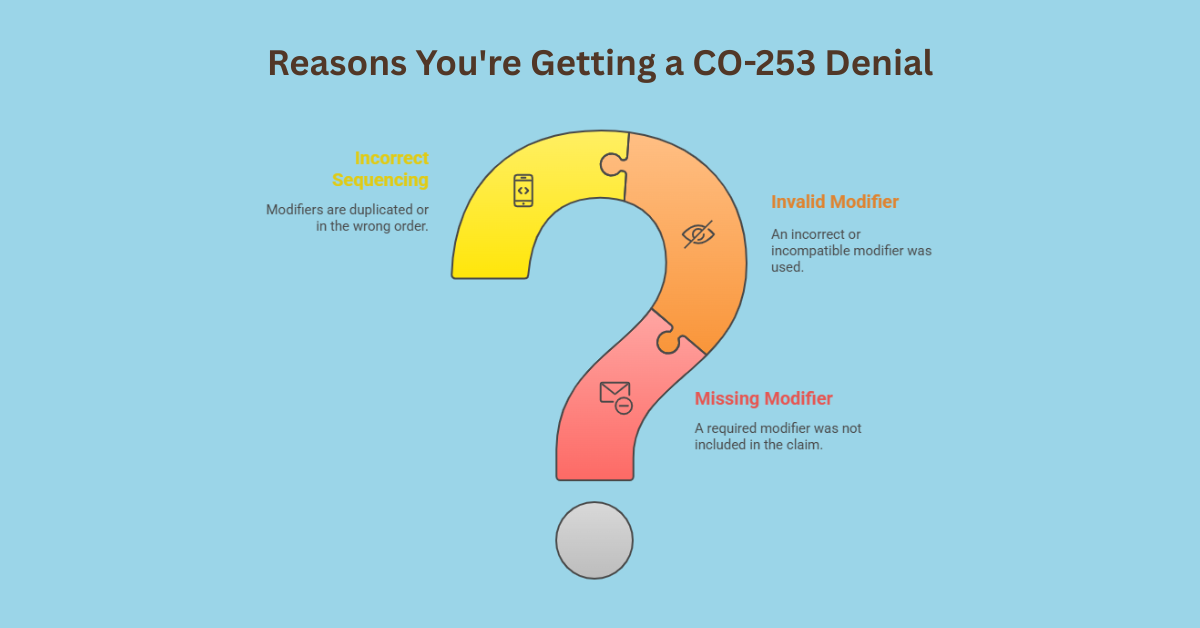
Top Reasons You’re Getting a CO-253 Denial
Fixing the CO-253 denial code starts with a precise diagnosis of the error. Here are the most common scenarios that trigger this denial.
A Required Modifier is Missing
Sometimes, the procedure code mandates the use of a specific modifier to provide context. For example, certain surgical procedures require a modifier to indicate which side of the body was operated on. If you forget to append the correct modifier, the claim will be incomplete and denied as CO-253.
You Used an Invalid or Incompatible Modifier
This is a frequent culprit. You might have used a modifier that simply does not make sense with the procedure code. For instance, appending a bilateral procedure modifier to a code that is inherently unilateral. The payer’s system sees this as an illogical combination and rejects it.
The Modifier is Duplicated or Incorrectly Sequenced
While less common, errors in the order of multiple modifiers or accidental duplication can also cause a CO-253 denial. Payers process claims based on very specific formatting rules.
Step-by-Step Action Plan to Fix CO-253
When a claim comes back with a CO-253 denial, do not panic. Follow this systematic approach to get it corrected and resubmitted.
Step 1: Conduct a Thorough Review of the Claim
First, pull the original claim. Carefully examine the procedure code and every modifier you submitted. Cross-reference this with the patient’s encounter form and the provider’s notes to verify what service was actually performed.
Step 2: Consult Payer-Specific Guidelines
Next, you must check the specific billing rules for that insurance payer. Do not assume all payers follow the same rules. Visit the payer’s provider portal and look for their:
-
Modifier Policy
-
Billing Manual
-
Code-Specific Bulletins
These documents will explicitly state which modifiers are acceptable for which codes.
Step 3: Verify Correct Coding with Authoritative Sources
After checking the payer’s rules, double-check your coding against standard references. The CPT Manual from the AMA and the National Correct Coding Initiative (NCCI) Edits from the CMS are your best friends here. The NCCI Edits, in particular, have a comprehensive table that shows which code-modifier combinations are allowed.
Step 4: Correct the Claim and Resubmit
Once you have identified the error, take corrective action.
-
If a modifier was missing, add the correct one.
-
If a modifier was invalid, remove it or replace it with the correct one.
-
If the sequencing was wrong, reorder them properly.
Then, resubmit the corrected claim. In most cases, you will need to send a new claim (electronically or on paper), not a claim appeal, since this was a correctable error.
Step 5: When and How to File an Appeal
Sometimes, you may find that your original coding was, in fact, correct according to the guidelines, but the payer’s system still denied it. In this rare case, you should file a formal appeal. Your appeal letter should be professional and include:
-
A copy of the Explanation of Benefits (EOB) with the denial.
-
Screenshots or excerpts from the payer’s own policy or the NCCI Edits that support your code-modifier combination.
-
A clear, concise explanation of why the claim was billed correctly.
Proactive Strategies to Prevent Future CO-253 Denials
The best way to manage the CO-253 denial code is to stop it from happening in the first place. Implement these proactive measures in your practice.
Invest in Ongoing Coder Education
Your billing staff must stay current with coding updates. Annual training on CPT and HCPCS code changes, including new modifiers, is not a luxury; it is a necessity. Consider bringing in an external expert for specialized modifier training.
Leverage Advanced Claim Scrubber Software
Modern billing software often includes advanced “claim scrubbers.” These systems run your claims through a series of automated edits before they are submitted to the payer. A good scrubber will flag potential CO-253 errors, allowing you to correct them in real-time and avoid the denial altogether.
Create and Use a Payer-Specific Modifier Cheat Sheet
As you work with different payers, you will notice patterns. Create a simple internal document or spreadsheet that lists common procedures your practice performs and the specific modifiers each major payer requires for them. This becomes a quick-reference guide for your billing team, saving time and reducing errors.
Frequently Asked Questions (FAQs)
Can I just remove the modifier to fix a CO-253 denial?
Only if the modifier was incorrect and not required. Often, the solution is to replace it with the correct modifier, not simply remove it. Removing a required modifier will likely cause a different denial or underpayment.
How long do I have to resubmit a claim after a CO-253 denial?
Timeliness is critical. You typically have the same filing deadline from the original date of service to resubmit a corrected claim. This is often 90 to 365 days, but you must check each payer’s contract to be certain.
Is a CO-253 denial the same as a contractual obligation?
No. A contractual obligation denial means you have agreed not to bill the patient. A CO-253 denial is a coding error that you can correct and resubmit for payment. After correction, the payer is obligated to process it.
Why did I get a CO-253 denial for a modifier that worked with a different payer?
Different insurance companies adopt and interpret coding guidelines differently. A modifier that is perfectly acceptable for Payer A might be considered invalid for the same code with Payer B. This is why checking payer-specific guidelines is so important.
What is the most common modifier mistake that leads to CO-253?
One of the most common errors involves the misuse of anatomical modifiers (like LT for left side, RT for right side) with codes that are already defined as bilateral or unilateral. Another frequent error is using an incompatible modifier for E/M services.