If you work in medical billing, you know that sinking feeling. You open the remittance advice and see it: the CO-24 denial code. This single code, meaning “charges not medically necessary,” can feel like a final judgment from your payer. But what if I told you that a CO-24 denial is often not a dead end, but rather a starting point for a conversation?
After over a decade in healthcare revenue cycle management, I have seen countless practices leave money on the table because they misunderstand this specific denial. They treat it as a write-off instead of a resolvable issue. This guide will change that for you. We will dive deep into what the CO-24 denial code truly means, why it happens, and how you can build a bulletproof process to fight it and prevent it from happening again. Let’s transform this common frustration into a manageable part of your workflow.
What is a CO-24 Denial Code, Really?
Let’s cut through the jargon. In plain English, the CO-24 denial code is your insurance payer saying, “The clinical information you sent us doesn’t convince us that this service was needed for this patient’s diagnosis.”
It is crucial to understand that this is an informational denial. The payer is not necessarily saying the service was frivolous. They are stating that the proof you provided with the claim—primarily the ICD-10 diagnosis codes—did not meet their specific criteria for medical necessity. Think of it as a failed audition; the performance (the service) might have been great, but the script (the documentation) didn’t fit the part.
CO-24 vs. CO-253: Knowing the Difference is Power
Many billing teams get tripped up by confusing CO-24 with other denial codes, especially CO-253. Mixing them up means you are applying the wrong solution, wasting precious time and resources.
-
CO-24 (Charges not medically necessary): This is a clinical and documentation problem. The link between the patient’s diagnosis (ICD-10 code) and the service you provided (CPT code) is too weak in the payer’s eyes. The battle is won with better clinical notes.
-
CO-253 (Procedure code inconsistent with modifier): This is a pure coding and billing error. The problem is a technical mistake on the claim form itself, like using an incompatible modifier with a procedure code. The fix happens in your billing software.
In short, CO-24 is about the ‘why,’ and CO-253 is about the ‘how.’ Correctly identifying the denial is your first critical step toward a resolution.
The Root Causes: Why You Keep Seeing CO-24 Denials
Understanding the “why” behind the CO-24 denial code is half the battle. These denials typically stem from a few common breakdowns in the process.
Insufficient or Vague Documentation in the Medical Record
This is the number one culprit. The provider’s notes might be brief, lack detail, or fail to paint a clear picture of the patient’s condition. For instance, a note that simply says “back pain” without describing the severity, duration, or impact on daily life provides little justification for an advanced imaging study like an MRI.
Mismatched ICD-10 and CPT Codes
Your billing team might be submitting a claim with a diagnosis code that does not directly support the procedure code according to the payer’s policies. For example, billing for a screening service without the appropriate preventive medicine diagnosis code can trigger a CO-24 denial. Payers use stringent systems like National Coverage Determinations (NCDs) and Local Coverage Determinations (LCDs) to define these relationships.
Missing or Inadequate Prior Authorization
Sometimes, you may have obtained prior authorization, but the service you performed deviated from what was approved. Alternatively, the authorization might have been for a different scope of service or number of units. The payer’s system will flag this discrepancy as not medically necessary.
Falling Behind on Payer-Specific Policy Updates
Insurance payers frequently update their medical necessity policies and covered diagnoses. What was perfectly acceptable six months ago might be denied today. If your practice is not proactively monitoring these changes from each major payer, you are essentially flying blind and inviting CO-24 denials.
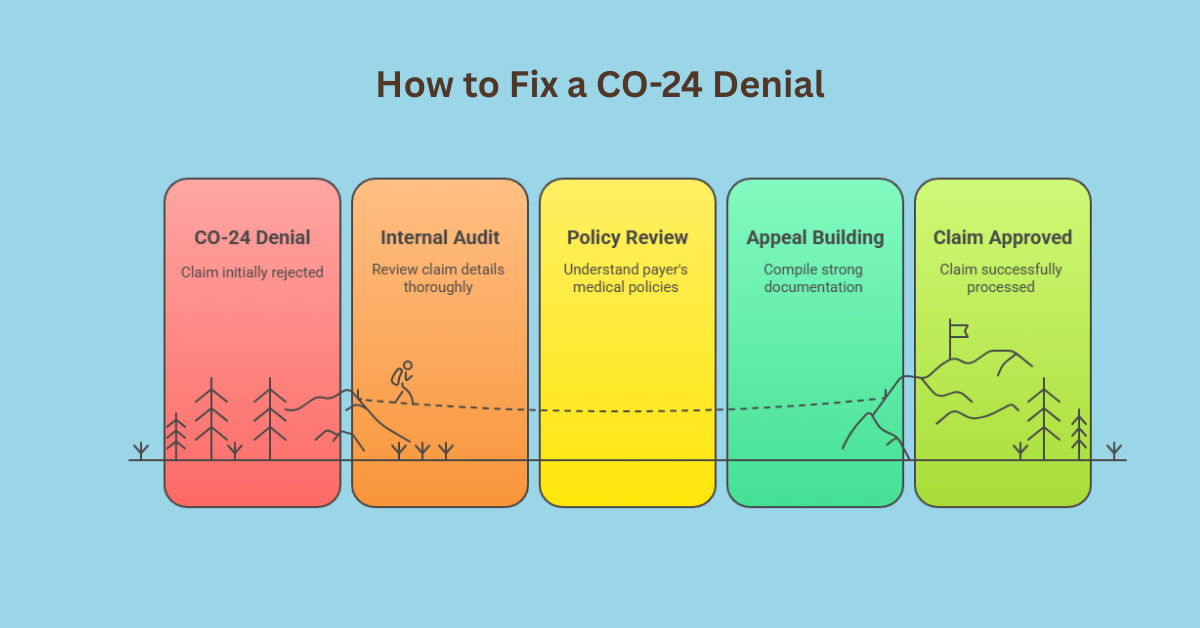
Your Action Plan: How to Fix a CO-24 Denial
When a CO-24 denial hits your desk, follow this structured, step-by-step approach to mount an effective response.
Step 1: Conduct an Immediate Internal Audit
Do not just look at the denial and resubmit the claim. First, gather all relevant documents:
-
The original claim (CMS-1500 form)
-
The patient’s full medical record for that encounter
-
The payer’s EOB/ERA with the CO-24 denial code
-
Any prior authorization documents
Your goal is to perform a gap analysis. Compare the clinical notes against the billed codes. Ask yourself: “If I were the payer, would this documentation convince me?”
Step 2: Dive Deep into Payer Medical Policies
Next, you need to research the rules of the game. Go directly to the payer’s provider portal and search for their specific medical policy or coverage determination for the CPT code in question. This document will explicitly list the ICD-10 codes and clinical scenarios they consider medically necessary. This is your roadmap for building a successful appeal.
Step 3: Build a Powerful Appeal with Robust Documentation
An appeal for a CO-24 denial is not about arguing; it is about educating the payer. Your appeal packet should be a compelling, self-contained story. It must include:
-
A Formal Appeal Letter: Clearly state the claim number, patient details, and date of service. Politely but firmly state that the service was medically necessary and provide a bullet-point summary of your supporting evidence.
-
Relevant Clinical Records: Do not send the entire chart. Highlight and attach the specific portions of the medical record that justify the service. This includes the history of present illness, physical exam findings, test results, and the assessment and plan.
-
Payer Policy Evidence: If applicable, include a snippet from the payer’s own medical policy that supports your case.
-
Supporting Literature: In complex cases, including a relevant clinical study or guideline from a recognized medical society can add significant weight.
Step 4: Submit and Meticulously Track the Appeal
Submit your complete appeal packet through the payer’s designated channel (often a specific portal or address) and be sure to note the deadline. Keep a detailed log of the submission date, the expected response time, and any follow-up communication. Persistence is key.
Proactive Prevention: Stop CO-24 Denials Before They Start
The ultimate goal is to prevent the CO-24 denial code from appearing in the first place. Shift your focus from reactive appeals to proactive prevention.
Implement Robust Clinical Documentation Improvement (CDI)
Work with your providers to enhance the quality of their notes. Encourage them to be specific, detailed, and to explicitly link the patient’s symptoms and findings to the medical decision for ordering a test or procedure. Templates can help, but they must be used to guide thorough documentation, not replace it.
Conduct Pre-Visit Payer Policy Checks
For scheduled procedures, make it a standard practice for your front-end staff to check the relevant medical policy before the patient arrives. This allows you to:
-
Confirm medical necessity in advance.
-
Secure the correct prior authorization.
-
Alert the provider if their planned procedure does not meet the payer’s criteria, allowing for a potential change in plan or a proactive peer-to-peer review.
Invest in Ongoing Coder and Biller Education
Your billing team must understand the nuances of medical necessity. Regular training sessions on ICD-10 coding specificity, payer policy updates, and the principles of correct coding initiative (NCCI) edits are a worthwhile investment that pays for itself in reduced denials.
Frequently Asked Questions (FAQs)
Can I bill the patient for a service denied as CO-24?
Generally, no. If the service was not medically necessary according to the payer, you typically cannot shift the cost to the patient unless you had them sign a valid Advance Beneficiary Notice of Noncoverage (ABN) before providing the service. Always check your payer contract.
How is CO-24 different from PR-2?
CO-24 is the “reason” code (why it’s denied). PR-2 is the “responsibility” code (who is responsible). PR-2 means “payer responsibility,” but it is often used in conjunction with CO-24 to indicate that the payer is not responsible for payment due to lack of medical necessity.
What is the timeline for appealing a CO-24 denial?
This varies by payer, but it is often tight, typically ranging from 30 to 180 days from the date of the initial denial. You must check the payer’s provider agreement for their specific appeal deadlines, as missing them can void your right to appeal.
Should I just write off small CO-24 denials?
This is a business decision, but be cautious. Writing off small denials might seem efficient, but it creates a hidden cost and ignores a systemic problem. If one small claim was denied for CO-24, others likely will be too. Addressing the root cause saves more money in the long run.
What is the most effective part of a CO-24 appeal?
The most critical component is specific, relevant clinical documentation from the medical record. The appeal letter guides the reviewer, but the clinical notes are the evidence that wins the case. Without strong documentation, your appeal is based on opinion, not proof.